-
PDF
- Split View
-
Views
-
Cite
Cite
Andrew Simmelink, Christopher Polk, Bevin Hearn, Gerald Capraro, A Nontraumatic Surprise Neck Mass, Clinical Infectious Diseases, Volume 63, Issue 7, 1 October 2016, Pages 991–992, https://doi.org/10.1093/cid/ciw415
Close - Share Icon Share
(See page 959 for the Photo Quiz.)
Diagnosis: Mucormycosis.
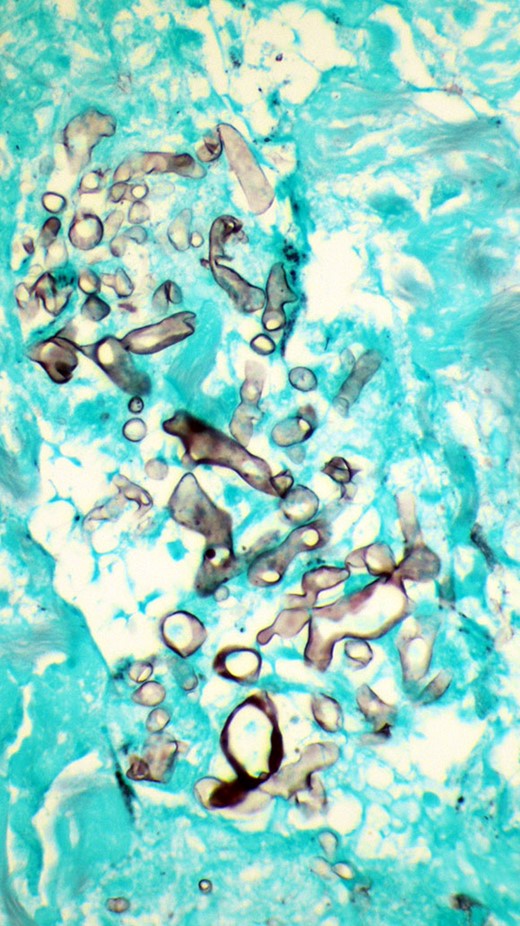
Histology revealed suppurative granulomatous inflammation, with numerous aggregates of fungal hyphae that appeared degenerated, but broad, ribbon-like, and pauciseptate (Figure 1). Impression was for Zygomycetes infection, and tissue submitted for culture subsequently grew Mucor species.
Grocott methenamine silver stain of surgical culture, showing numerous aggregates of fungal hyphae that appeared degenerated, but broad, ribbon-like, and pauciseptate, 400x magnification.
Mucormycosis is often a rapidly progressive disease with high mortality approaching 30% in some series. This infection most commonly presents with rhinocerebral and pulmonary disease in hosts with diabetes or following solid organ and bone marrow transplants. Cutaneous mucormycosis (Figure 2) is less common and described most frequently in patients suffering trauma from combat or natural disasters such as tornadoes or tsunamis [1]. In many case reports, cutaneous mucormycosis appears to progress more slowly than classically described rhinocerebral [2] and pulmonary forms. Cutaneous mucor has been reported in both immunocompetent and immunocompromised hosts. Our patient did not have a history of neck trauma but did have subacute presentation.
Mucor infection is rare in patients with AIDS. In a retrospective study of 1630 autopsies of AIDS patients from 1984 to 2002, Antinori et al observed only 2 patients with mucormycosis [3–5]. Another case series reviewing mucormycosis in human immunodeficiency virus (HIV)–infected patients in the pre–highly active antiretroviral therapy (HAART) era found only 15 cases [6, 7]. In the post-HAART era, the few case reports of mucormycosis in HIV-infected individuals involve patients with coexistent immune deficits from solid organ transplant or lymphoma [8, 9]. In HIV-infected patients, Mucor has been most commonly described with pulmonary and renal disease [6, 7].
Management of mucormycosis includes source control with surgical debridement, oftentimes requiring multiple procedures, and antifungal therapy [10]. First-line therapy includes amphotericin deoxycholate or liposomal amphotericin B at 5–10 mg/kg until clinical recovery, which can take weeks of treatment [11]. Of note, amphotericin lipid complex formulation is inferior therapy unless combined with an echinocandin, and therefore other amphotericin formulations are preferred [12]. Alternative or step-down therapy includes posaconazole or isavuconazole [13]. Additionally, any underlying immunocompromise should be corrected, if possible.
Our patient's initial surgical debridement was thought to be adequate, and he was initiated on liposomal amphotericin at 5 mg/kg daily for a 2-week course. He clinically improved with less pain and edema, and repeat radiographic studies demonstrated a considerably smaller abscess cavity without any cervical adenopathy. He was discharged on oral posaconazole 200 mg 3 times daily with plans for a prolonged duration of therapy. He was also initiated on HAART with abacavir-lamivudine-dolutegravir in a fixed-dose combination.
Note
Potential conflicts of interest. C. P. reports personal fees from ViiV Healthcare, and grants and personal fees from Gilead Sciences. B. H. reports grants from Gilead, Merck, ViiV Healthcare, and Bristol-Myers Squibb. All other authors report no potential conflicts. All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.





Comments